What’s MVP Got to Do With It?
As early as the 19th century during wartime, soldiers were presenting with a “condition” of:
- Chest discomfort
- Rapid pulse
- Dizziness
- Faintness
- Shortness of breath with or without exertion
- Palpitations
- Fatigue
- A range of digestive complaints
Amazingly, these first patients, soldiers, had normal physical exams. Da Costa noted the condition often followed a period of hard service in the field, a febrile illness or battle wounds; however, he also reported that several soldiers had a history of similar symptoms before enlisting. At that time soldiers were treated with prolonged bed rest rest and digitalis. Over 100 years later and we are still talking about the “condition” that is afflicting and robbing men and women of their quality of life. The names given to the “condition” have changed since the 1800’s but the “condition” has not.
Over time this “condition” has been called by various names including Soldier’s Heart, Da Costa’s Syndrome, Neurocirculatory Asthenia, muscular exhaustion of the heart, Effort syndrome, irritable heart, mitral valve prolapse, mitral valve prolapse syndrome and now Dysautonomia which is probably the most accurate term anyone could give to date. This is a very broad category sometimes called an umbrella term encompassing many different problems under its covering.
Over 35 years ago, the founder of the first clinic in Birmingham, Alabama was cardiologist Dr. Phillip Watkins. He called the clinic The Mitral Valve Prolapse Center. It was a very simple start as he began to see more and more patients with what was called at that time Mitral Valve Prolapse. At that time technology allowed us to view the heart with a special ultrasound called an echocardiogram. Dr. Watkins as well as many of his colleagues noted Mitral Valve Prolapse in many patients who also had a very particular constellation of symptoms. They are almost identical to those reported by Da Costa over 100 years ago.
MVP involves prolapse of one of the valves of the heart, the mitral valve.
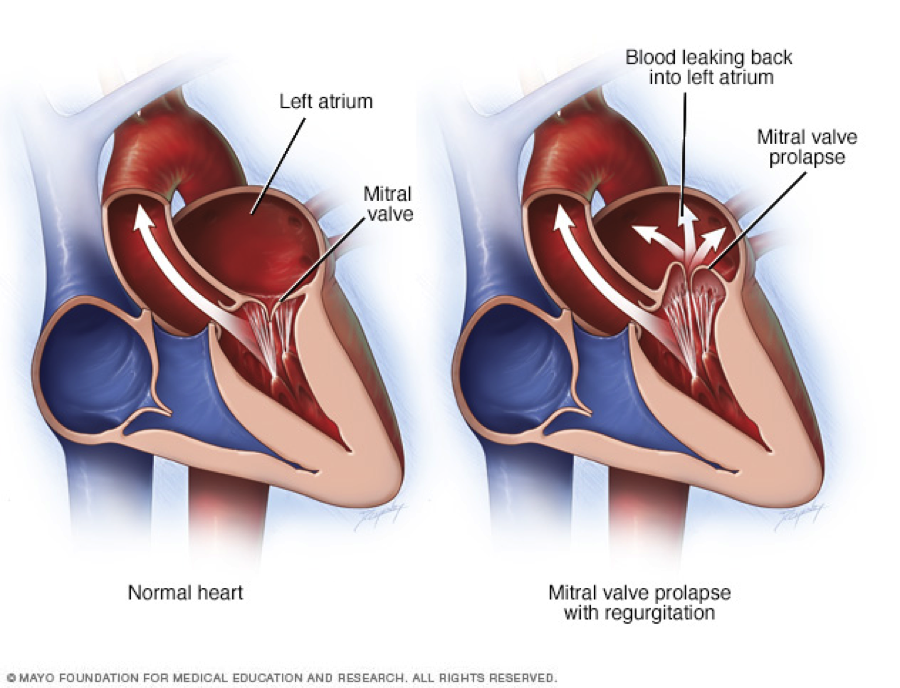 The mitral valve sits at the opening between the left atrium and left ventricle, and opens and closes so that blood flows only in one direction (left atrium to left ventricle). In MVP, the mitral valve fails to make a proper snug fit, and instead billows (prolapses) back into the atrium. There is also a sound described as a click that can be heard through a stethoscope.
The mitral valve sits at the opening between the left atrium and left ventricle, and opens and closes so that blood flows only in one direction (left atrium to left ventricle). In MVP, the mitral valve fails to make a proper snug fit, and instead billows (prolapses) back into the atrium. There is also a sound described as a click that can be heard through a stethoscope.
In most people, mitral valve prolapse isn’t life threatening, does not cause symptoms and does not require treatment or changes in lifestyle.
Sometimes, however, the mitral valve fits so poorly that a large amount of blood leaks back from the left ventricle to the left atrium. This is called “mitral regurgitation,” and if severe it can be dangerous, eventually requiring surgery.
MVP can develop in any person at any age. Sometimes MVP runs in families because of certain genetic disorders such as Marfan’s Syndrome, Ehlers-Danlos Syndrome, Muscular Dystrophy or Scoliosis.
The name changed to Mitral Valve Prolapse Syndrome because it was felt that MVP did not cause the symptoms but was present in many patients with MVP.
However, recent evidence indicates that symptoms of Dysautonomia occur with no greater frequency in people with MVP than in people without MVP. In other words, there is probably no connection between the two conditions. People who were previously diagnosed with MVP Syndrome are now said to have two separate conditions: MVP plus symptoms of Dysautonomia.
Dr. Phillip Watkins set his life’s mission to help these people who have what we now know to be Dysautonomia with POTS making up the largest subset of my patients. I am forever grateful for the 20 years I was able to spend with this pioneer in the Dysautonomia world. He was my boss, my colleague and my friend. He is greatly missed by his many patients who’s lives he changed. He is greatly missed by me.
